What Small Businesses Need to Know About the Employer Mandate
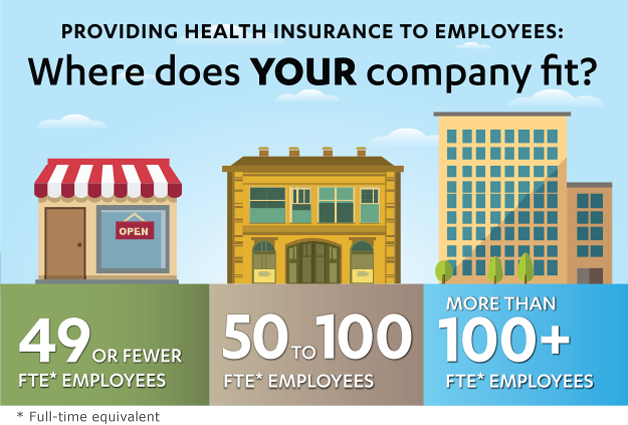
Under the Affordable Care Act (ACA), businesses with 50 or more full-time equivalent (FTE) employees that do not offer health coverage, or that offer health coverage that does not meet certain minimum standards, may be subject to a financial penalty, referred to as the Employer Shared Responsibility payment. The Employer Shared Responsibility provisions, often referred to as the “employer mandate,” have been in effect since 2015 for businesses with 100 or more FTE employees. But, starting in 2016, the employer mandate will become effective for businesses with 50 or more FTE employees. The purpose of this summary is to provide a brief overview of the employer mandate provisions, and to inform your business about how you may be impacted by changes to the provisions made in 2016.
Overview of the Employer Mandate
Starting in 2016, the employer mandate will be enforced for businesses with 50 or more FTE employees. A business may have to pay a per-employee, per-month fee called the Employer Shared Responsibility Payment if the business:
- Does not offer coverage (to at least 95 percent of FTE employees) that complies with specified reforms under the Affordable Care Act.
- Does not offer coverage that meets minimum value. (The plan’s share of the total average cost of covered services is at least 60 percent).
- Does not offer coverage that is affordable. (The employee’s premium is more than 9.66 percent of that employee’s annual household income).
If a business does not offer coverage, the Employer Shared Responsibility Payment penalty is triggered when an employee who is not offered coverage purchases health insurance on an exchange and receives a federal subsidy to help pay for that coverage. The penalty is assessed monthly and is equal to the number of FTE employees (minus the first 30) multiplied by one-twelfth of $2,000.
If a business offers coverage, but that coverage does not meet minimum-value and affordability requirements, the penalty is triggered when an employee rejects offered coverage and purchases health insurance on an exchange and receives a federal subsidy to help pay for that coverage. The payment is assessed monthly and is the lesser of: one-twelfth of $3,000 per FTE employee receiving federal subsidies through the exchange, or one-twelfth of $2,000 per full-time employee (minus the first 30).
I'm an Employer
Information on setting up health insurance for small business